Event Overview
The 2024 Medicare Provider Enrollment Compliance Conference (MPECC) is presented by Eide Bailly with special guest speakers from the Centers for Medicare & Medicaid Services’ Provider Enrollment and Oversight Group.
MPECC will feature in–depth guidance on enrolling as a Medicare provider and/or supplier, maintaining enrollment privileges, and the associated compliance risks. This event also provides direct access to CMS officials, representatives from all the Medicare Administrative Contractors (MACs), multi–state, regional contractors responsible for administering both Medicare Part A and Medicare Part B programs, and PECOS-designated stations directly outside the meeting space with representatives from CGI Federal to assist with your questions.
You can anticipate an invaluable, educational three-and-a-half days, which will include:
- Keynote sessions
- Panel discussions
- Special guest speakers
- Most up-to-date guidance and changes to Medicare provider enrollment
- Direct access to CMS officials, representatives from the Medicare Administrative Contractors (MACs), and the PECOS development contractor
Important links:
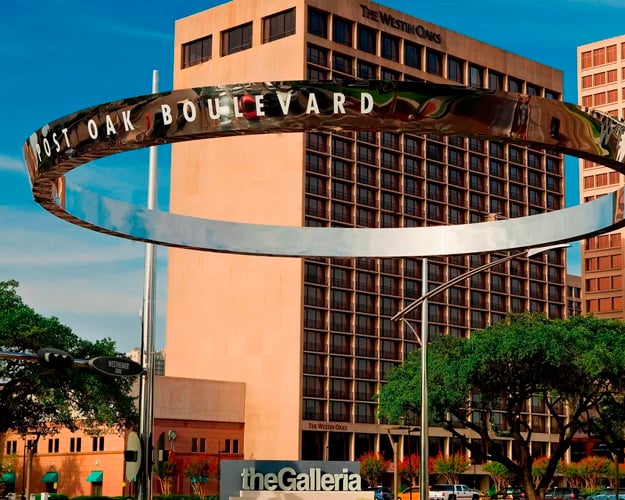
- RESERVE HOTEL ROOM (Deadline to book: February 5, 2024)
- VIEW CONFERENCE AGENDA
 Dennis Grindle CPAPartnerFor more than 36 years, Dennis has worked with healthcare clients across the country on Medicare provider enrollment (Form CMS-855 completion and compliance), Medicare provider enrollment appeals, Medicare provider-based regulations, Medicare reimbursement issues, physician and non-physician practitioner Medicare billing rules, licensure and related issues.
Dennis Grindle CPAPartnerFor more than 36 years, Dennis has worked with healthcare clients across the country on Medicare provider enrollment (Form CMS-855 completion and compliance), Medicare provider enrollment appeals, Medicare provider-based regulations, Medicare reimbursement issues, physician and non-physician practitioner Medicare billing rules, licensure and related issues. Gretchin Heckenlively CPA, FHFMAPartnerSince 1997, Gretchin has specialized in providing healthcare consulting, Medicare and Medicaid provider enrollment, provider-based reimbursement and billing services. She is a recognized thought leader in the healthcare industry and has given numerous presentations on a wide range of healthcare-related topics at a local, state and national level.
Gretchin Heckenlively CPA, FHFMAPartnerSince 1997, Gretchin has specialized in providing healthcare consulting, Medicare and Medicaid provider enrollment, provider-based reimbursement and billing services. She is a recognized thought leader in the healthcare industry and has given numerous presentations on a wide range of healthcare-related topics at a local, state and national level.- Zabeen ChongDirector, CMS Provider Enrollment and Oversight GroupZabeen Chong serves as the Director for the Provider Enrollment and Oversight Group in the Center for Program Integrity at CMS. Zabeen is responsible for leading initiatives to streamline provider screening and enrollment for over two million providers and implementing policies and systems to prevent fraud and abuse in the Medicare and Medicaid programs. This includes the development of Medicare and Medicaid provider enrollment operating policy and procedures, enumeration of provider applicants, oversight of the Provider Enrollment Chain & Ownership System, and providing outreach and education to the provider community. She is also responsible for the identification of vulnerabilities and implementation of administrative action processes directed at protecting Medicare and Medicaid provider enrollment. Prior to her current position, she served as the Director of the Website Project Management Group in the Office of Communications at CMS where she led the redesign and implementation of new technologies onwww.medicare.gov and www.cms.gov as well as other web-based initiatives critical to advancing CMS’ mission and operations. Zabeen has a Master’s degree in Information Technology from the Johns Hopkins University and has worked at CMS for over 15 years.
- Charles SchalmDeputy Group Director, CMS Provider Enrollment and Oversight GroupCharles Schalm has been serving as the Deputy Director for the Provider Enrollment & Oversight Group at the Center for Program Integrity at CMS since 2013. He is responsible for overseeing the federal screening, enrollment, and enforcement actions for 2.7 million providers and suppliers that serve over 65 million Medicare beneficiaries. Prior to joining CMS, Charles served in the private sector as a Program Integrity Director for Medicare and Medicaid fraud, waste and abuse. He also worked with Medicaid managed care organizations in Pennsylvania and Michigan. He served on the national Medicare/Medicaid Healthcare Drug Taskforce where federal agencies and private organizations came together to tackle the onset of the opioid epidemic. Charles went to school at the University of Michigan and Duquesne University, where he graduated with degrees in business and forensics.
- Alisha SandersDirector, Division of Enrollment Policy & Operations, CMS Provider Enrollment and Oversight GroupAlisha Sanders serves as the Director for the Division of Enrollment Policy & Operations within the Provider Enrollment and Oversight Group in the Center for Program Integrity at CMS. Ms. Sanders is responsible for developing enrollment policies and procedures across the Medicare program and working with the Medicare Administrative Contractors (MACs) and other stakeholders on provider enrollment and program integrity related issues. Ms. Sanders has over 20 years of experience in Medicare provider enrollment.
- Vani AnnadataDirector for the Division of Enrollment Systems, CMS Provider Enrollment and Oversight GroupVani Annadata serves as the Director of the Division of Enrollment Systems within the Provider Enrollment and Oversight Group in the Center for Program Integrity at CMS. She is responsible for overseeing the National Medicare Provider Enrollment System (PECOS), the National Plan & Provider Enumeration System (NPPES) and the provider enrollment screening system. Vani has been with CMS for over twelve years. She has an extensive background in software and systems development for over 15 years in private sector and holds a degree in Engineering.
- Allison BloomDeputy Director for the Division of Enforcement Actions, CMS Provider Enrollment and Oversight GroupAllison Bloom serves as the Deputy Director of the Division of Enforcement Actions within the Provider Enrollment and Oversight Group in the Center for Program Integrity at CMS. She is responsible for overseeing and developing policy surrounding the implementation of administrative actions, including enrollment denials, revocations, and deactivations of provider’s Medicare billing privileges. Allison has a BS from The Pennsylvania State University and has been with CMS for 8 years.
- Adam Rubin, Esq.Adam Rubin serves as a senior technical advisor in the Provider Enrollment & Oversight Group in the Center for Program Integrity at CMS. He is responsible for assisting in the development of new program integrity regulations and statutes to further bolster CMS’s mission of curbing fraud, waste, and abuse in the Medicare and Medicaid programs. Prior to joining CMS in 2016, Adam practiced as an Estates and Trusts attorney in Towson, MD. As a certified mediator, he has mediated workplace disputes under the umbrella of the Federal Shared Neutrals program. Adam received his J.D. from the University of Maryland Francis King Carey School of Law.
- Joseph SchultzDeputy Director for the Division of Enrollment Policy and Operations, CMS Provider Enrollment and Oversight GroupJoseph Schultz serves as a Deputy Director of the Division of Enrollment Policy and Operations within the Provider Enrollment and Oversight Group in the Center for Program Integrity at CMS. Mr. Schultz is responsible for developing enrollment policies and working with the Medicare Administrative Contractors (MACs) and other stakeholders on provider enrollment and program integrity related issues. He has over 13 years’ experience in Medicare for both the public and private sector. Joseph has a Master’s degree in Healthcare Administration from Utica College in NY and undergraduate degree from the State University of New York at Cortland.
- CPE Credits30.5 - View the agenda to see the complete CPE details
- Field Of StudySpecialized Knowledge
- Level Of KnowledgeOverview
- Delivery MethodGroup Live